
Lilly Tague-Bleau tested positive for Covid-19 nearly six months ago, and yet the effects of the virus continue to plague her.
The 16-year-old New Hampshire junior contracted Covid in June while working her after-school job as an aid at a nursing home. While she didn't end up in the hospital during the roughly two weeks she was sick with the worst of the infection, she's also not fully recovered yet. She suffers from what's called post-Covid syndrome, and struggles with extreme fatigue, headaches and rapid heartbeat.
"It's a little bit isolating sometimes because it's not a common shared thing. It's not relatable," Tague-Bleau tells CNBC Make It.
Like Tague-Bleau, there are tens of thousands of people in the U.S. who are suffering from post-Covid syndrome, also known as long haulers. And it's not just the elderly who are impacted.
There's a growing number of younger Americans experiencing the effects of Covid, with cases among Gen Z, millennials, Gen X and younger baby boomers starting to spike over the summer and continuing apace into the winter months. As of Nov. 18, Americans between the ages of 18 and 39 accounted for about 40% of the total U.S. cases of the Covid-19 cases tracked by the Centers for Disease Control and Prevention.
And many of those who contract Covid aren't recovering quickly. One British study found that about 10% of Covid patients have lingering symptoms, and many of the youngest long haulers are worried how these ongoing health complications could impact their futures. In many cases, those suffering from long-term issues are fighting multiple battles: Not only are they struggling to fully recover their health, but they're also grappling with increased medical costs and uncertainty around their futures after contracting the virus.
Cases are on the rise, but understanding of long-term effects of Covid still a black box
Money Report
Those who test positive for Covid and have symptoms generally recover within two to four weeks, says Dr. Greg Vanichkachorn, an occupational medicine specialist at the Mayo Clinic who is currently working to create a rehabilitation program specifically for Covid-19 patients struggling with lingering effects from the virus.
Those suffering from post-Covid syndrome, however, are still persistently experiencing symptoms on a daily basis four weeks after the acute infection phase, Vanichkachorn tells CNBC Make It. Most frequently, those lingering symptoms include fatigue, shortness of breath, headaches and "brain fog," where patients find it difficult to concentrate.
"We still don't know yet how it's going to affect [patients] long term," Vanichkachorn says.
The majority of these long haulers are younger patients, says Dr. Noah Greenspan, a cardiopulmonary physical therapist and founder of the New York-based Pulmonary Wellness and Rehabilitation Center and the new Covid Rehabilitation and Recovery Clinic.
Yet some of these cases may be a result of how the public has been told to manage their Covid symptoms, Greenspan says. "At no other time in [modern] history would you see a patient with 103-degree fever who is having difficulty breathing, told not to go to the emergency room, told instead to shelter at home, ride it out," he says.
And the question is, for many of these long haulers, had they been admitted, had their blood pressure been monitored around the clock, their heart rate and rhythm monitored, their blood checked — would they still be dealing with long-term health complications?
"We don't know," Greenspan says. "But I think there's definitely something to that. Hopefully in the future, as we get better at managing this, we'll see less and less long haulers over time."
"Covid is like nothing I've seen. It's almost like we're learning everything from scratch, feeling our way around in the dark," Greenspan adds.
Financial costs of ongoing symptoms can add up
Corianne Goldstein, 32, contracted Covid very early on in the pandemic, around the second week of March. Her case proved to be more serious, and she was admitted to a hospital in New Jersey on March 17 and ultimately spent more than a week there.
At one point, her doctors wanted to place Goldstein on a ventilator. "They came back with the latest test and basically said to me, we have to get you on a vent probably tomorrow. Make sure that you talk to your family and say goodbye because you'll be sedated and vented and you won't be able to speak," Goldstein recalls. "But I didn't do that because I was terrified."
Fortunately, Goldstein's test results improved the next day and continued to improve, with her fever finally breaking nearly two weeks after the initial onset of symptoms. And yet, she's still struggling with the effects of the virus today.
Goldstein says she still regularly experiences "brain fog" where she loses her train of thought and struggles with forgetfulness, as well as having ongoing issues with stamina. Prior to Covid, she took barre class four times a week and did cardio, but now she can't exercise at anywhere near that level.
Perhaps more troubling, Goldstein's blood thickened because of Covid, which has caused her heart to pump harder, and she's still struggling to breathe normally. When she left hospital, Goldstein had a pulse oxygen level of 80%, yet that's only recovered to about 85%. Normal oxygen levels are at least 95%.
And with every trip to a specialist or doctor, the costs increase. Goldstein is lucky to have insurance and only had to pay around $1,000 of the roughly $140,000 bill for her hospital stay and treatment. Yet there are still doctor's appointments and tests that continue to add up, including appointments with cardiologists, neurologists and pulmonologists.
A Covid patient with insurance who requires a hospital stay is billed an average of $38,221 for care. But consumers typically only pay a portion of that bill, usually the cost of their health plan's deductible, which averaged $1,931 for a single employee in 2019, according to the Kaiser Family Foundation.
Tague-Bleau, who is on her mother's insurance, estimates her family has spent between $200 and $400 out-of-pocket for her care, which includes driving roughly 100 miles round trip to Boston Children's Hospital up to three times a month to see specialists there. In a typical year, Tague-Bleau says she'd only spend about $50 in copays.
"I can't imagine how much they would have would have charged had we not had insurance. That's really been the saving grace. I don't think we would have even gone to the doctors had we not had insurance," Tague-Bleau says.
There are certainly extra costs involved, agrees Cat Tague, Lilly's mother. And it's not just the direct medical costs, but also indirect costs such as time, as well as as gas and parking expenses involved in driving to Boston. "Instead of having the day together to do some fun things, we're hauling now to Boston to get lots of testing done. That's exhausting," she says.
Covid long haulers worry about what the future holds
Yet, it's the potential future costs and implications that worry Goldstein the most. "If Covid does make your blood thicker, and it makes your heart pump harder, is that something that makes your life expectancy lower? Is that something that affects you long term?" she questions.
It's still too early to know the potential long-term costs associated with contracting Covid, but research shows that there's a significant difference in health costs between people who have chronic conditions and those who don't.
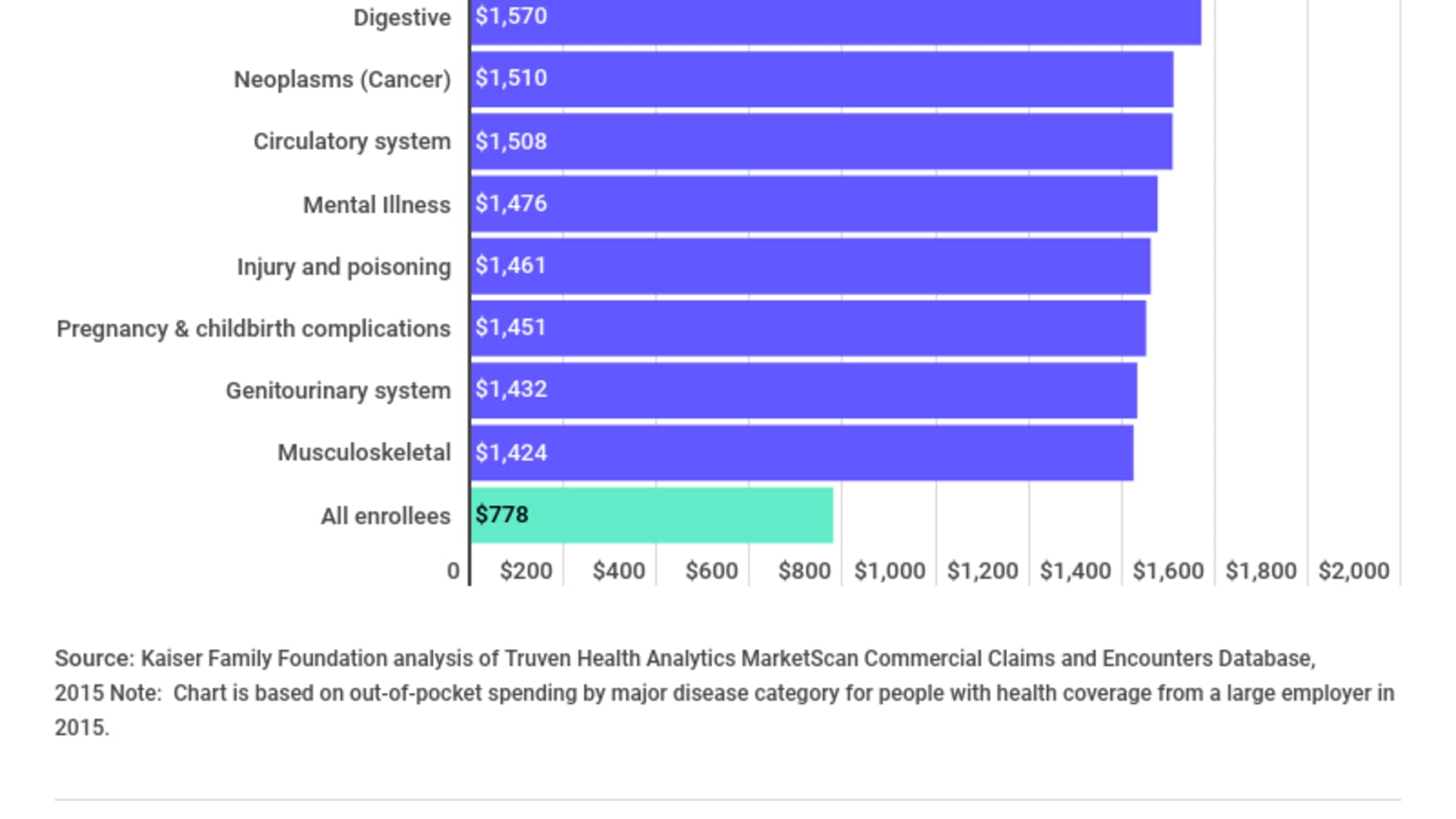
Diseases of the blood, congenital anomalies and circulatory system diseases are among the most expensive chronic conditions for patients under the age of 65, adding up to average out-of-pocket costs over $1,500 annually, though blood diseases average closer to $2,000, according to Kaiser. Meanwhile the average health insurance plan participant without a chronic condition pays just $778 a year out-of-pocket.
Roughly 1 in 5 Americans ages 18 to 49 have been diagnosed with at least three chronic conditions that do not affect their ability to function normally, according to research from the Commonwealth Fund. Unsurprisingly, these adults typically visit the doctor and hospital far more than the average American. And that leads to higher healthcare spending — about $905 out-of-pocket annually among patients with multiple chronic conditions, compared to $445 spent by the average American in the same age range.
Concerns extend beyond the cost of care
Covid long haulers aren't just worrying about long-term healthcare expenses. There's also the opportunity costs: If they are facing a lifelong illness, how will their futures be impacted?
Before Covid, Tague-Bleau was an active student athlete. While she rejoined her field hockey team this fall, she struggled to explain her illness to her teammates. "They thought that I was infecting people. I got a bunch of calls from teammates, from coaches," she says. "There was just this weird alienation for a little bit where people stood a little further away once they knew I'd had Covid, even though it was a couple months ago."
Tague-Bleau also worries about her grades and college prospects. "It's made learning so much more difficult," she says, adding that her school has been operating remotely this fall, which has made it even harder to focus. "Being on remote all day long has been really detrimental to my grades. And I'm thinking well, maybe I can't go to this college or do this career. It's only based on one year, but still it's kind of throwing a wrench in [my goals]."
The experience has changed her mother's outlook on the virus as well. "I wasn't as worried or concerned. But after what she went through with that experience, it definitely made me recognize that folks who think this doesn't have any impact on someone so young and healthy are wrong. It does," Tague says. "This is not something you want your kids to get, no matter how young and healthy they are."
For Goldstein, she's concerned about her plans for starting a family. "I'm 32, and my husband and I just got married two years ago. We were supposed to be trying for a baby and starting in May," she says. But there are a lot of uncertainties now around not only the effects of Covid on fertility, but also all of the antibiotics and medications that Goldstein was given to help her recover. She's currently seeing a fertility specialist, but no one has any real answers.
"That makes me nervous," Goldstein says. "Covid, in my experience, is and will continue to be with me every day and part of every decision I make. Every time I have a shortness of breath or every time my heart's beating too hard, I'll think about how it has affected, me and if this is something that can potentially impact my life long term."
Don't miss: Best credit cards for Black Friday and Cyber Monday shopping of 2020
Check out:






