Experts say the end of the coronavirus pandemic state of emergency could have a big impact on those of us who may have gotten used to having access to certain COVID-related health benefits. Here's what you should know about how your health care could be affected by the end of the emergency declaration on May 11.
Will COVID-19 tests be free?
COVID-19 tests at-home and in labs may not be free for you any longer. The public health emergency required insurers to reimburse for up to eight at-home tests per month, and free testing at the doctor's office. But after Thursday, you may have to pay for those. Check with your health plan for details. However, for those of you on Medicaid, you will continue to get free testing through September 2024.

Get San Diego local news, weather forecasts, sports and lifestyle stories to your inbox. Sign up for NBC San Diego newsletters.
What about Vaccines?
Now, you may wonder what will happen with the COVID-19 vaccines? Free coverage is required for all vaccines recommended by the CDC, so these will continue to be no cost to you, as long as you use an in-network provider.
"There’s no one right now who cannot get a free vaccine or booster," said Cynthia Cox, vice president at Kaiser Family Foundation. "Right now all the vaccines that are being administered are still the ones purchased by the federal government."
NBC 7 Responds
But the Biden administration has said it is running out of money to buy up vaccines and Congress has not budged on the president's requests for more funding.
Can I get COVID-19 treatments once the emergency ends?
Finally, treatments for COVID-19, such as Plaxlovid, will also remain free as long as those doses have been purchased by the federal government. When that supply has finished, the price will be determined by the manufacturers.
Will Medicaid be Affected?
Medicaid enrollment ballooned during the pandemic, in part because the federal government prohibited states from removing people from the program during the public health emergency once they had enrolled.
The program offers health care coverage to roughly 90 million children and adults — or 1 out of every 4 Americans.
Late last year, Congress told states they could start removing ineligible people in April. Millions of people are expected to lose their coverage, either because they now make too much money to qualify for Medicare or they've moved. Many are expected to be eligible for low-cost insurance plans through the Affordable Care Act's private marketplace or their employer.
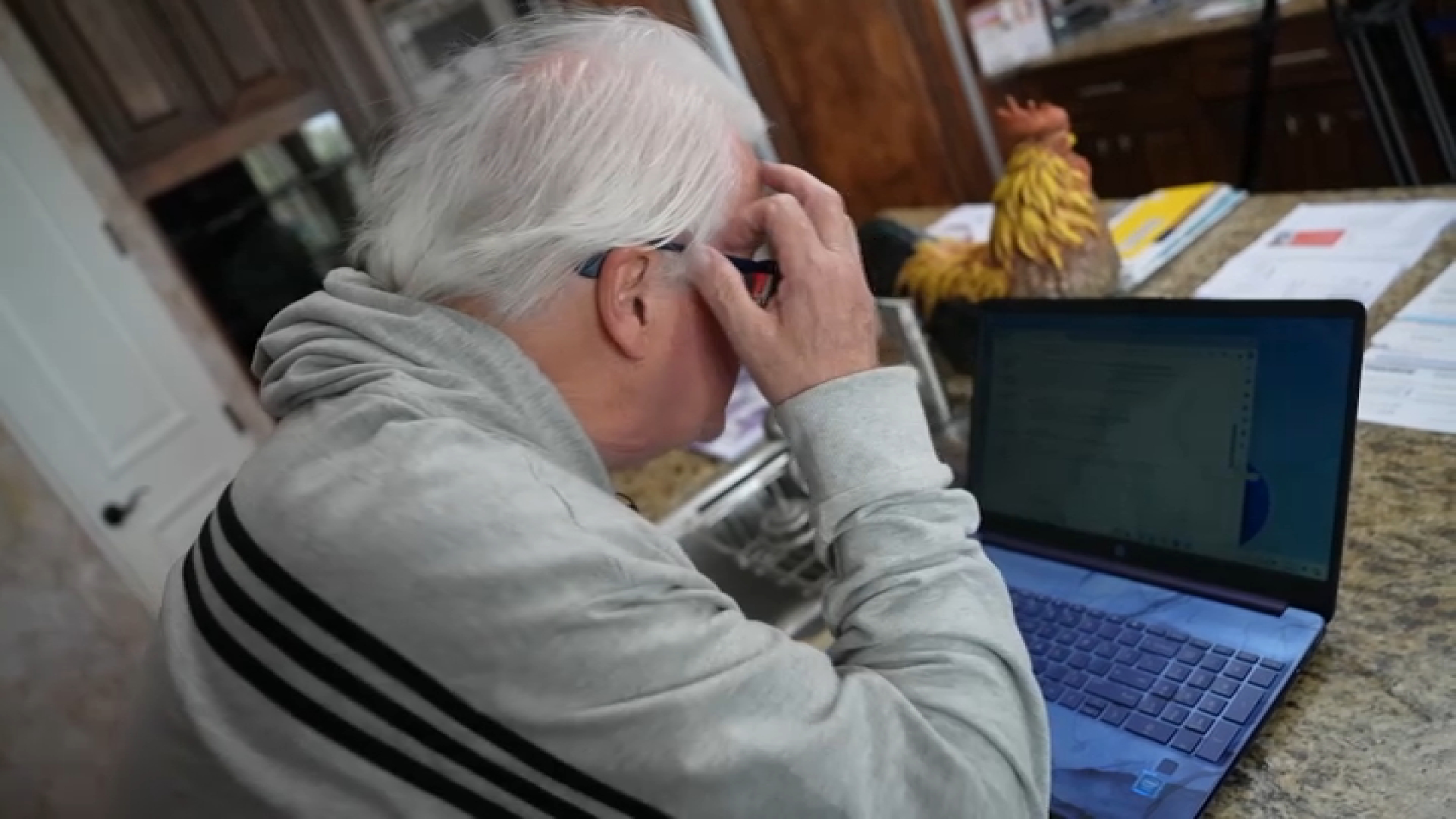
Can I still get a Telehealth visit?
COVID-19's arrival rapidly accelerated the use of telehealth, with many providers and hospital systems shifting their delivery of care to a smartphone or computer format.
The public health emergency declaration helped hasten that approach because it suspended some of the strict rules that had previously governed telehealth and allowed doctors to bill Medicare for care delivered virtually, encouraging hospital systems to invest more heavily in telehealth systems.
Congress has already agreed to extend many of those telehealth flexibilities for Medicare through the end of next year.
Money for Hospitals
Hospitals will take a big financial hit in May, when the emergency comes to an end. They'll no longer get an extra 20% for treating COVID-19 patients who are on Medicare.
The end to those payments comes at a time when many hospitals are under financial pressure, struggling with workforce shortages and dealing with the pain of inflation, said Stacey Hughes, the executive vice president at the American Hospitals Association.